If you are a parent, grandparent, babysitter, or just someone who spends time around infants, then you need to know how to perform infant CPR. Infant CPR is a life-saving technique that everyone should know how to do, and it is especially important for those who care for infants on a regular basis.
Infant CPR courses are available at many community colleges, hospitals, and Red Cross offices. The American Heart Association (AHA) recommends that everyone should learn CPR, even if they do not have young children. You never know when you may be called upon to save a life. Refresher CPR courses are also a good idea for those who have not had training in a while.
The Basics Of Infant CPR – How To Perform It On A Baby Who Is Not Breathing.
Infant CPR is a life-saving technique that everyone should know how to do. If you are ever in a situation where an infant is not breathing, it is important to know how to properly perform CPR. Here are the basics of performing infant CPR:
- Position the baby on its back on a firm surface. If you are worried about hurting the baby’s spine, you can place your hand on the forehead and gently tilt the head back while supporting the jaw with your other hand.
- With the heel of your hand, give 30 chest compressions at a rate of 100-120 per minute.
- Place your mouth over the baby’s mouth and nose and blow two rescue breaths, each lasting one second.
- Continue with 30 chest compressions and two rescue breaths until help arrives or the baby starts showing signs of life, such as coughing or crying.
If the baby starts coughing or crying, they are still in danger and you should continue to monitor them closely as they may stop breathing again. It is also important to call 911 even if the baby appears to be okay.
When And Where Should You Use Infant CPR?
You should use infant CPR any time an infant is unresponsive and not breathing properly. This includes if they are gasping for air, if they have stopped breathing altogether, or if they are only making sporadic gasping noises. Additionally, if an infant has been submerged in water for more than 20 seconds, you should begin performing CPR even if they appear to be breathing normally.
It is also important to know that Infant CPR can be used anywhere – whether you are at home, at the park, or even in the car. As long as there is a flat surface available, you can perform Infant CPR.
What Are The Risks And Benefits Of Performing Infant CPR On Someone Else’s Child Or Your Own Child If They Are Choking Or Not Breathing?
There are some risks associated with performing Infant CPR, particularly if the person performing it has never been trained in how to do it properly. For example, if chest compressions are done too hard, it could potentially break ribs or damage internal organs. Additionally, if rescue breaths are not given correctly, it could force air into the stomach instead of the lungs which could cause vomiting and aspiration (inhaling vomit into the lungs).
However, despite these risks, Infant CPR can be extremely beneficial – even lifesaving – when performed correctly and in a timely manner. According to the American Heart Association (AHA), “for every minute that passes without [CPR], survival rates decrease by 7-10%.” Therefore, it is always better to attempt Infant CPR than to do nothing at all.
How Can You Get More Information About Infant CPR, Including Taking A Class In Your Area?
The best way to learn Infant CPR is by taking a class from a certified instructor. However, there are also many online resources available that can provide helpful information about how to perform Infant CPR. Additionally, most hospitals offer free classes periodically throughout the year. You can also check with your local Red Cross chapter for more information about upcoming classes. Learning Infant CPR could one day save a life – so it is definitely worth taking the time to learn!
Conclusion
CPR can be the difference between life and death for an infant. When performed correctly, it can help to restart the heart and lungs and get oxygen flowing to the brain. Time is of the essence when performing CPR, so it is important to know how to do it properly. If you have never been trained in CPR, or it has been a while since your last refresher course, don’t hesitate to sign up for one today! It could one day save a life.
Check other Courses:
Adult-Child-Infant CPR/AED & First Aid Training
Adult CPR/AED & Standard First Aid Training
Adult-Child-Infant CPR/AED Training
Online Adult, Child, Infant CPR Classes & First Aid Training
Online First Aid Course & Certification
Online First Aid Course Canada
Check out our other CPR & First Aid Related Articles:
INFANT CPR CERTIFICATION & ITS IMPORTANCE
THE IMPORTANCE OF TAKING BLS TRAINING
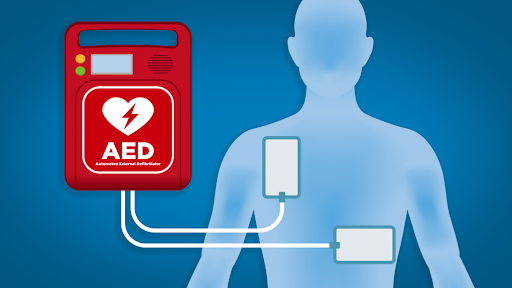
WHAT IS THE DIFFERENCE BETWEEN CPR AND AED TRAINING?
WHEN TO USE A MANUAL OR AUTOMATIC EXTERNAL DEFIBRILLATOR
10 THINGS YOU DIDN’T KNOW ABOUT CPR
THE AMERICAN HEART ASSOCIATION OR RED CROSS: WHICH IS BEST FOR CPR CERTIFICATION?
4 WAYS TO PREPARE BEFORE YOU LEARN HOW TO GET A FIRST AID CERTIFICATE
CPR TRAINING FOR EVERYONE: WHY IT IS IMPORTANT